Traditional Disc Replacement Surgery
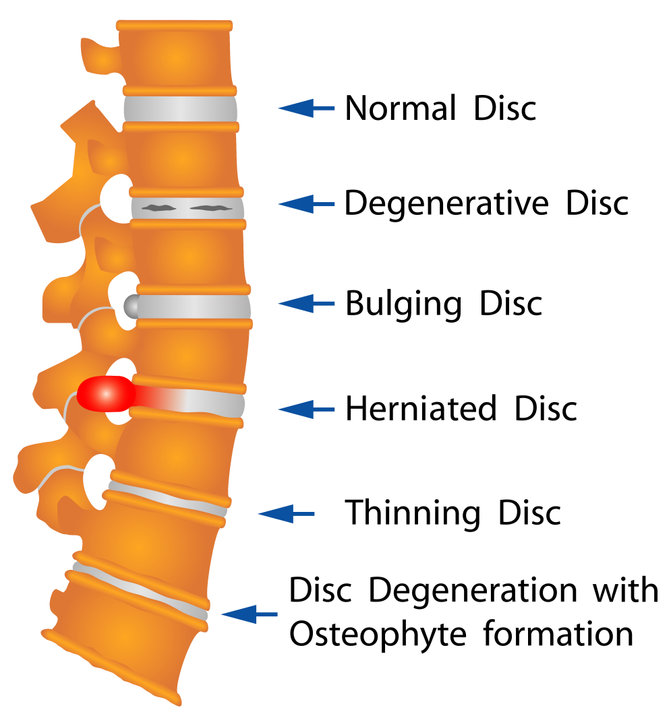
As we age, the discs in our spine begin to flatten and wear down, bringing the vertebrae closer together. This can put added stress not only on the disc but also on the surrounding joints, muscles, and nerves. This process is known as disc degeneration and can lead to several painful conditions including disc herniation and bone spurs.
To determine if the disc is the reason for your pain, a discogram may be performed. For this test, a small amount of fluid is injected into the disc space and the pressure within the space is gradually increased. The examiner will ask you if you are experiencing pain while the pressure is increased. If this reproduces your typical pain, the test is positive at that level. This process is repeated at each disc space that is suspected of causing pain, plus one additional disc space, which is used as a control, meaning you should not experience pain at this level.
What is Disc Replacement Surgery?
During a disc replacement surgery, an intravenous line (IV line) is placed into your arm and you will be placed under general anesthesia, which includes a tube, also known as an endotracheal tube, placed down your throat to help you breathe. In the cervical spine, a small incision is made on the front of your neck, to the left of your windpipe, to access your cervical spine. In the lumbar spine, a team of surgeons including a general surgeon and an orthopedic spine surgeon, work together to make an incision on the belly and form a channel through the abdominal wall to the spine. The surgeon may use retractors or other tools to create a channel from the skin to the spine, allowing access to the disc space.
Next, the disc material is removed from the disc space and the affected nerve root is relieved of pressure. An implant is inserted into the disc space using specialized instruments and the wound is closed. This implanted device will imitate the functions of a normal disc and allow patients to regain a normal range of motion and quality of life.
Similar to any major surgery, you should expect some discomfort and to go through a period of post-surgery rehabilitation. Depending on the procedure performed and the patient, you may go home the same day from the hospital or surgery center or stay overnight in the hospital. Typically, the use of postoperative pain medications is minimal, and walking in the postoperative period is encouraged. Before your procedure, you will be given instructions on what you can and can’t do after the procedure. Likely, you will be asked to avoid all activities that involve repeated or extreme bending, twisting, pushing, pulling, and lifting.
Who is a Candidate for Disc Replacement Surgery?
Many conditions can result in back pain, but not all back pain comes from the vertebral disc. Your primary care provider can begin the process of determining where your back pain is coming from and can also start a trial of conservative treatment. When back pain is severe and/or is not well-managed with conservative methods, consultation with a spine surgeon is likely the next step.
New advancements in spine surgery have provided the option for artificial disc replacements in the neck or lower back. These implants include M6-CⓇ and Mobi-CⓇ for the neck and ActivLⓇ for the lower back. Currently, the M6-CⓇ implant is only FDA-approved for a single-level fusion, but the Mobi-CⓇ and ActivLⓇ implants are FDA-approved for single or multi-level disc replacements.
Strong candidates for a cervical or lumbar disc replacement surgery have:
- Back pain isolated to the disc space of 1 or 2 levels
- No significant disc space narrowing
- No significant facet joint-related disease or pain
- No bony compression on a nerve
- A healthy body weight
- No history of osteoporosis, spinal deformity, or scoliosis
- No previous major back surgery in that area
However, each patient is unique. Proper examination, imaging, and/or other tests should be completed to allow the spine specialist to determine whether an artificial disc replacement is the right option for you.
Benefits of an Artificial Disc Replacement vs. Fusion
- Maintain the range of motion of the spine. In many patients, motion is significantly decreased due to pain or stiffness before surgery. A disc replacement returns normal disc space height and provides normal motion, causing many patients to notice an increase in motion following surgery. With a fusion, motion is prevented at that disc space.
- Reduced stress on the spine. With a disc replacement, motion is maintained and the disc space height is returned to normal, reducing stress on the surrounding disc spaces, joints, and ligaments. With a fusion, motion is removed at one or more disc spaces. This increases stress on the disc spaces above and below the fusion, worsening the wear and tear on those discs.
- Faster recovery. Minimally invasive surgery results in a faster recovery time. Smaller incisions, less blood loss, less risk of infection, and less damage to surrounding structures, result in a shorter recovery. With a fusion, activities are limited for a longer period to allow for bone healing and a proper fusion.
Disc replacement surgery can provide many short and long-term advantages. As always, it is best to discuss your options with a spine specialist to decide what is best for your situation. Find out if a disc replacement is an option for you. Schedule a consultation or contact us today.
For more information on an artificial disc replacement versus a spinal fusion, check out this video.
