What is Spinal Stenosis?
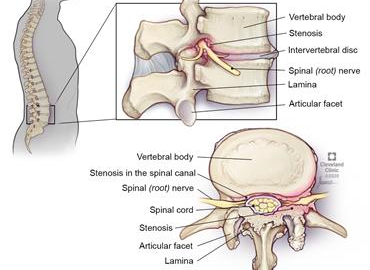
Spinal stenosis is the narrowing of the spinal canal. As people age, their discs dry out and collapse or herniate. The body stiffens the spine by thickening the spinal ligaments, hardening the disc, and forming bone spurs.
Unfortunately, these changes can result in a narrowing of the spinal canal and compression of the spinal cord, nerve roots, and/or blood vessels. The compression on the nerve irritates that nerve, resulting in pain in that area of the spine and along the course of that nerve. The brain thinks the arm or leg is the cause of the pain when it is the pressure on the nerve in the back or neck.
Lumbar vs. Cervical Stenosis
The types of spinal stenosis are classified according to where the condition occurs. Although it is possible to have more than one type of stenosis, the two main types are lumbar stenosis and cervical stenosis. Lumbar stenosis is narrowing in the lower back, while cervical stenosis is narrowing in the neck area. These are further classified by the specific area that is narrowed. For example, if the narrowing is within the foramen, the area where the nerve exits the spine, this is called foraminal stenosis. If the narrowing is around the spinal canal, this is called central canal stenosis. And, if the narrowing is in between these two areas, this is called lateral recess stenosis.
Diagnosing Spinal Stenosis
An MRI or CT scan is necessary to diagnose whether your symptoms are attributable to spinal stenosis; however, it is not the sole determining factor. It's important to recognize that the presence of spinal stenosis in your imaging does not automatically imply it is the source of your symptoms. It is not uncommon to have spinal stenosis findings without experiencing any symptoms. Your provider will conduct a comprehensive assessment, including an examination and a review of your symptom history, to ascertain whether this finding is pertinent to your symptoms and requires treatment.
Alternate causes for arm or leg pain can be peripheral neuropathy or a referred pain. Peripheral neuropathy is when the nerves outside of the spine can be damaged. Examples of peripheral neuropathy are carpal tunnel syndrome or diabetic neuropathy. Referred pain is when the pain is felt in a part of the body other than the location of the source of pain.
Symptoms of Spinal Stenosis
Cervical Stenosis Symptoms
- Numbness or tingling in the arm, hand, or fingers
- Weakness in the arm, hand, or hand
- Headaches
- Neck pain
Lumbar Stenosis Symptoms
- Numbness or tingling in a foot or leg
- Weakness in a foot or leg
- Pain or cramping in one or both legs when walking or standing stationary for long periods that is relieved with sitting or bending forward
- Back pain
If your spinal cord is being compressed due to central canal stenosis, you may experience various symptoms depending on the location in the spine. This can include numbness, tingling, and/or weakness in the extremities, balance issues, difficulty with hand dexterity, or bowel/bladder dysfunction.
Treatments for Spinal Stenosis
Treatment for Spinal Stenosis depends on the severity of symptoms and the location of the stenosis.
Medications
If medications are the best treatment for your situation a doctor may prescribe anti-inflammatories, pain relievers, muscle relaxants, antidepressants, or opioids.
Physical Therapy
At the onset of spinal stenosis, it is common for people to become less active to reduce the pain. But, less activity will lead to muscle weakness resulting in more pain. Physical therapy may be prescribed to help build muscle strength, maintain flexibility and stability of the spine, and improve balance.
Steroid Injections
While steroid injections do not fix or reverse the stenosis, they can reduce inflammation of the nerve which can resolve the pain.
Spinal Decompression Surgery
If symptoms are severe and other treatments have proven ineffective, surgery may be the best option. Like other treatments, surgery is meant to decompress the area and resolve the symptoms of spinal stenosis. Depending on the cause of stenosis, a small portion of bone, ligament, and/or disc material may be removed. Spinal stenosis can be treated by different surgical approaches and discussing your situation with an experienced surgeon, like Dr. Hanson, will reveal what procedure is best for your case.
To find out if your symptoms are a result of nerve compression, schedule a consultation today!
